Value at your desk. Contact Us
Last June 24, 2021, the Food and Drug Authority issued a public health warning on three cosmetic products:
1. The Ordinary Niacinamide 10% + Zinc 1% High-Strength Vitamin and Mineral Blemish Essence
2. The Ordinary AHA 30% + BHA 2% Peeling Solution
3. The Ordinary Hyaluronic Acid 2% + B5
The FDA issued Advisory No.2021-1543 warning the public to avoid purchasing the said skincare products because of failure to undergo through the agency’s registration process. Without undergoing proper registration and validation, FDA cannot assure the public on the products quality and safety.
The Food and Drug Administration (FDA) warns the public from purchasing and using the unauthorized cosmetic products.
Read more:-> https://bit.ly/3eDHjj1
By Aznaida L. Tawagon-Pandapatan, MD, DPDS
What are Retinoids?
Retinoids are Vitamin A derivatives. Use of retinoids results to the most sought-after reversal of skin aging.
How? By organized differentiation and proliferation of skin cells. Think of it as like an organic fertilizer for plants—once applied to the soil, the leaves and fruits will grow faster and with a better quality.
When applying retinoids, skin cells will grow faster and better (like how your skin used to be when you were younger) and collagen will start to form in your skin dermis, so you can get back that youthful smooth, firm, and glowing skin.
Currently there are four generations of retinoids:
Naturally-occurring: Retinol & Retinaldehyde
Synthetic: Tretinoin, Isotretinoin, and Alitretinoin
What are their uses?
Retinoids are most famous as anti-acne and anti-aging, but amazingly in the medical field, they are also used for other diseases such as in psoriasis, hyperkeratotic conditions and even for cancers. Here we discuss their anti-acne, anti-aging, and anti-melasma actions.
Retinoids have been used for acne vulgaris (pimples) since 1971. Topical Tretinoin & Adapalene are the preferred retinoids for acne.
These retinoids do their superhero work by normalizing the follicular epithelial differentiation, thus treating the existing pimples and also preventing future pimples to form. New studies also showed that topical retinoids have an anti-inflammatory activity thus further decreasing pimple occurrence.
Adapalene causes less irritation compared to tretinoin, thus it is commonly prescribed for those with sensitive skin and those who cannot tolerate Tretinoin.
Retinols are milder forms of retinoids. Examples are retinaldehyde & retinyl palmitate. These may be advised for those who cannot tolerate the use of Adapalene & Tretinoin. Studies showed satisfactory results with these retinols, although effects can be slower and milder compared to adapalene and tretinoin.
Oral Isoretinoin (tablet form) is prescription-only and is used for moderate to severe acne that cannot be successfully controlled by creams. Therapy usually lasts for 6 months, and when acne has been controlled, this is shifted by your Dermatologist to topical retinoids as maintenance.
As anti-aging, Tretinoin has been shown to give superior results overall. Fine wrinkles and brown spots are the two targets of retinoids as anti-aging.
Brown spots or Dyspigmentation], which happens in photoaging, can be treated by retinoids, partially or fully, depending on how severe it is. This is through enhancement of proper cell turn-over of the epidermis, thus shedding off of the darkened/damaged skin cells on top.
Wrinkles can be improved by retinoids by enhancing cell regeneration of the topmost skin layers and by production of new collagen in the dermal layer (lower layer of the skin). This effect on collagen can usually be observed after 6-12 months of regular use.
Melasma has 3 types: EPIDERMAL (affecting the topmost skin layers), DERMAL (affecting lower skin layer), and MIXED epidermal+dermal (affecting both the top and lower layers).
Epidermal type of melasma can be improved by retinoids by enhancing regeneration of new skin cells, thus effectively removing the topmost pigmented cells. Improvement can be 80-100%.
In Mixed type of melasma, the epidermal component can be treated by retinoids by the same mechanism mentioned above, but the lower dermal component does not usually respond to this. Thus the patient can only see a partial improvement of their melasma, about 50-60% improvement.
Dermal type of melasma is difficult to manage with just topical retinoids, it is managed with multiple approaches using lasers and other topicals.
Retinoids can be combined with other treatment modalities to optimize melasma treatment.
What are the possible side effects of retinoids?
Like many medications, retinoids may have side effects, some are mild and some are severe especially for the first-time users. Here are some of them:
Do not let these side effects turn you off from using retinoids. Most of these effects
will usually resolve on their own once the skin adjusts. But for those with severe side effects, your dermatologist will prescribe medications to lessen the effects and guide you when and how to re-introduce it to your regimen.
Tips on proper use of retinoids and how avoid undesirable effects.
Myths about retinoids in skincare:
Facts about retinoids in skincare:
References
Danielle Nicolle Dionisio Mejia, MD, DPDS
Martha Joy Bruan-Tapales, RPh, MD, FPDS
The science of prescribing medication is second nature to physicians. The therapeutic relationship between a patient and a doctor is founded in mutual trust that the patient will follow the regimen prescribed by the doctor. However, in therapeutics, there are unintended events that may occur anytime during treatment.
The World Health Organization (WHO) defines adverse drug reaction (ADR) or effect as an individual’s response to a drug which is noxious or unintended occurring at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease, or for modifications of physiological function. In addition, the US FDA describes it as an undesirable effect associated with the use of a drug that may or may not be related to its intended pharmacological action. In short, ADR is harm caused by the drug at normal dose during normal use.
The classification of ADRs can be divided according to the following:
Side effect, a type of ADR that is most commonly discussed with patients, is defined as the unintended and sometimes unavoidable effect occurring at normal dose related to the pharmacological properties. The drug’s side effects are usually listed down by the drug manufacturers for the physicians to know and relay to the patient. Examples of drug side effects would be hair loss and oral ulcers with the use of cancer medication; burning or stinging sensation with the use of topical retinoids or topical calcineurin inhibitors; nausea and vomiting with the intake of doxycycline. Since side effect is a response related to the pharmacological properties of a drug, some would include in the definition effects that are beneficial to the patient even though it is not the main aim of therapy.
Adverse drug reaction or adverse drug effect, therefore, is the umbrella term for all undesirable effects of a medication, whether it is expected or not and to some whether it is good or bad.
The long term safety of a drug can only be determined once it is being widely used by the public. Monitoring adverse drug reactions from medications is important to safeguard the public from these effects. Timely reporting of ADRs is vital and healthcare workers can not do this without the help of the public. Proper health education and efficient communication between the healthcare workers and patients is important to allow prompt monitoring of these unwanted drug related events.
References:
Tanya Perez-Chua, MD, FPDS
The topic Skin Care on a Budget is very interesting and tricky. Budget is always relative. What is affordable to you, may not be affordable to me. To make your budget work, I will also give advice on how to spend wisely. I have seen thousands of patients over the years and the following are my thoughts as a board-certified dermatologist and dermatopathologist.

Asking for the expert’s opinion will save you a lot of time, money and effort. Since they are highly trained, they will give you the most effective medications that may include oral, topical and even injections. There won’t be a need to try so many products. Everytime you purchase a new cream or supplement, you spend money and worse, you will get frustrated if you do not get your desired result. Spare yourself those and just consult a dermatologist. Make sure you are consulting a legit dermatologist. Professional fees vary. The Philippine Dermatological Society has training institutions that gives real treatment and proper prescriptions at professional fees that are almost for free!

So many products from all over the world are now very accessible to everyone. But remember, what is popular may not work for you. When we see advertisements, the photos and “feedback” are always impressive. However, you do not really know the truth behind these. Always think twice before grabbing another product.
I am not fond of cleansers with a lot of active ingredients. I only recommend special cleansers for those with severe cases of atopic dermatitis and other eczemas. For cases of pimples, I choose a simple soap or liquid cleanser – one that would not harm the skin. I do not depend on soaps and cleansers to cure pimples, dark spots, and scars.

It is a rule to always apply sunscreen. The dark spots on your face will not go away without protecting yourself from the skin. The wrinkles will continue to form faster because of the sun! If you want to age beautifully, the minimum requirement to achieve this is to put sunscreen. I do not like sunscreens that incorporate other active ingredients. Sometimes, these may even cause a contact dermatitis. As I always tell my patients, choose a simple and effective sunscreen.

I have noticed that a lot of consumers gravitate to goods that peel dramatically. I encounter these people when they go to my clinic and realize that the “peeling” actually burned their skin after using these products. I always warn my patients about these. Unfortunately, such strong products are also widely available in stores and online.
On the other hand, some over the counter products may work! Ask your dermatologist if they would approve of those. Yes, you may need some guidance in choosing over the counter products.

A simple skin regimen would not break the bank. A simple regimen will be effective and safe! I am also not a fan of having to apply so many things on our faces and bodies. A simple regimen may need oral medicines and you really have to consult your board-certified dermatologist for this.
When you have a skin problem that you think is hopeless or might be too expensive to treat, choose to consult a board-certified dermatologist! Do not waste your time and money buying so many products. We will talk and solve your skin concerns, keeping your budget in mind.

Dr. Aenelle B.Dizon FPDS
Caring for one’s skin is all about taking care of one’s self. It is not considered an indulgence but more of a necessity. The main goal of having a skin care routine is to maintain the skin’s function at its best, with no irritation or any signs of skin disease.
Before starting a skin care routine, it is important to identify and understand one’s skin type. This will help in one’s choice of products to use.
As dermatologists we agree that more is not always better and a basic skin care routine is as easy as a three-step procedure of cleansing, moisturizing and protecting.

CLEANSING – Washing the face is the most basic and essential step in any routine. Our skin is constantly exposed to pollutants, dirt, oil, make up and all of these should be gently removed. Washing the face two times a day (morning and night) is basic. Finding the right cleanser with the right formula is important. A product that is fragrance free, gentle and cleanses without stripping the essential moisture of the skin is ideal for everyday cleansing according to skin type. Here is a simple guide;
NORMAL skin – Soap free cleanser or a micellar water is suitable for most people with normal skin
OILY or Acne prone skin- Look for a foaming liquid with no added emollients and one which can decrease sebum from the skin
DRY skin – Look for cream cleansers that are formulated with emollients to help hydrate the skin
MOISTURIZING- Moisturizing the skin is an important step in a skin care routine. A moisturizer traps water in the skin and is best applied to damp skin at least 2 x daily. They can also complement the naturally protective oils within the skin. It is recommended to moisturize one’s skin regardless of skin type because the skin naturally loses its ability to retain moisture especially as we age. Or as we engage in daily activities such as washing the face frequently can strip off the natural moisture from the surface.
Here is a guide on how to choose a moisturizer according to skin type:
For OILY Skin – Choose a gel moisturizer, it is usually water based, lightweight and has quick absorption.
For DRY Skin – a cream moisturizer is ideal
For NORMAL Skin- Lotion form is the classic moisturizer level which absorbs well
PROTECTION – Protecting the skin with sunscreen is a crucial part of a skin care routine. Daily and consistent use of sunscreen helps to prevent fine lines, wrinkles, age spots and certain skin cancers. In choosing the ideal sunscreen look for a product that is broad spectrum which means it can provide protection from both UVA and UVB rays and with little risk of irritation or health concerns. It is recommended to use sunscreen with a minimum spectrum SPF of at least 30.
Sunscreen application 101
Apply sunscreen 30 minutes before sun exposure and re apply at least every two hours. Make sure to apply enough sunscreen to appropriately cover the entire face and exposed areas of the body
Besides the basic steps of cleansing, moisturizing and protecting additional extra steps can be done as needed. These are products which one can add to the basic skin care routine mentioned above. These can be in the form of toners, serum, exfoliants, or masks to target a more specific skin concern. A general rule of thumb I s to apply the products with thinner consistency underneath the thicker ones. Face masks can be used periodically not more than once or twice per week.
As you choose products for your skin care routine, stick to key, important active ingredients and avoid experimenting too much, be consistent and wait for the skin products to work on the skin by maintaining for at least 2-3 months. Except if it causes allergic or adverse reaction, then it is warranted to stop the product right away.
Consistency or doing the skin care routine regularly is key to having a good, well-maintained skin.
Reagan Grey T. Reyes, MD, DPDS
Board-certified dermatologists are known to be the leading experts when it comes to skin, hair and nails. While this is true, dermatologists are also aware and recognizable of sexually transmitted infections, which refer to a variety of infections that can be acquired and transmitted through sexual contact.
Because of their typical skin symptoms (genital discharge, ulcers, lumps/bumps, itchiness), dermatologists are the first line physicians who are sought after by patients with sexually transmitted infections (STIs). It is important to keep in mind that both the doctor and the patient play a critical role in preventing and treating these common STIs.
List of common STI’s in Dermatology according to symptom:
-Genital Discharge:
Diseases presenting with genital discharge may also present with burning and painful urination. Gonorrhea is caused by the bacteria neisseria gonorrhea, while chlamydia is caused by the bacteria chlamydia trachomatis. They are transmitted sexually and also from infected mother to child.
Chlamydia presents with a less profuse and less purulent discharge than neisseria. Both diseases are treated with oral antibiotic therapy. Recent sex partners within 60 days should be referred for testing and presumptive antibiotic treatment. Other causes of genital discharge in women include: bacterial vaginosis, trichomonas vaginalis and candidiasis.
-Ulcers:
Genital ulcers are either painful or nonpainful. Genital herpes, caused by herpes simplex virus 1 and 2, presents as recurrent, grouped, painful blisters, which eventually leads to ulcers. It is usually accompanied by fever, headache and/or body weakness. Primary syphilis, on the other hand, is caused by the bacteria Treponema pallidum, and will present as a painless ulcer, which may later on progress to form generalized rash, fever, joint pains and/or hair loss.
For genital herpes, it is treated with antiviral medications, while for primary syphilis, further work-up is needed to confirm the diagnosis and this is treated with antibacterial therapy. Other causes of genital ulcers that are uncommon include: chancroid, lymphogranuloma venereum and donovanosis.
-Lumps/bumps:
Lumps or bumps located in the genital, anal and/or pubic region may be caused by genital warts or molluscum contagiosum. HPV types 6 & 11 in 90% of cases, as well as other HPV types cause genital warts. Molluscum contagiosum, on the other hand, is caused by the pox virus, MCV.
These diseases are transmitted by direct person-to-person contact as well as through contaminated objects. It can also be transferred to other parts of the body by scratching or scraping the skin.
Treatment options include topical medications and modalities like extraction or excision, electrocautery, cryosurgery or chemical peels. Watchful waiting for spontaneous resolution is sometimes an option. Vaccines for genital warts caused by HPV are available and is given to patients as early as teenage years to provide maximum protection.
-Itchiness
Pediculosis pubis, caused by the crab lice Phthirus pubis, is a marker for STI risk and is transmitted through pubic apposition, sleeping in the same bed and with exchange of towels. Scabies, on the other hand, is caused by the ectoparasite Sarcoptes scabiei and is transmitted through prolonged skin-to-skin contact.
Persons with both diseases usually seek medical attention because of intense genital itchiness, which may be associated with skin lesions on the genitalia and intertriginous area. These diseases are treatable with topical and/or oral medications and treating family members and sexual partners is equally important.
-HIV/AIDS:
The spectrum of skin manifestations associated with HIV is vast. The skin is the largest and most visible organ of the body, and although the cutaneous immune system serves as the body’s first line of defense against infection, it can also present numerous cutaneous manifestations.
Nearly all individuals with HIV will develop a skin disorder at some point in their clinical course, some of which can be debilitating and disfiguring; these conditions may present challenges for both patients and clinicians hence the importance of recognition and management of HIV-related cutaneous manifestations. Consultation with your board-certified dermatologist and infectious disease specialist is a must in HIV patients presenting with skin disorders.
CONCLUSION
Despite the current pandemic situation, STI cases are still alarmingly on the rise. With that, vigilance is a must when it comes to these diseases. Complete STI screening is recommended for persons with symptoms of STI and that prevention through abstinence, being faithful, correct and consistent condom use, drug avoidance, and education, is vital in fighting these infections. Your board-certified dermatologist is trained in treating these infections and consultation is the first step and key for proper diagnosis and treatment.
References:
1. https://www.cdc.gov/mmwr/pdf/rr/rr6403.pdf
2. https://www.hiv.uw.edu/go/basic-primary-care/cutaneous-manifestations/core-concept/all
Pia Victoria Velasco MD, FPDS
Healthy skin entails adequate sun protection. Without sun protection, it increases our risk for sunburn, skin aging and even skin cancer.
Here are some practical tips on how to protect your skin from the sun:
Seek shade when appropriate. The sun’s rays are most intense between 10 am and 2 pm.
Another way to protect yourself from the sun’s harmful UV rays is by wearing protective clothing. Dermatologists recommend wearing the following:
Proper choice of clothing can provide some sun protection. When selecting what to wear, avoid fabrics with a loose or open weave such as lace. Likewise, dark colors offer more protection than light colors.
A wide brimmed hat is a simple way to provide additional protection for the face and neck. Avoid caps and straw hats with a loose weave.
When choosing sunglasses, read the label to determine if the lens will provide adequate sun protection. In addition, large-framed sunglasses would offer more protection as compared to smaller frames.
If you opt to wear sandals or flip-flops or go barefoot outdoors, be sure to apply adequate amounts of sunscreen on all exposed areas.
Apply a broad-spectrum sunscreen with an SPF of 30 or higher.
SPF stands for Sun Protection Factor. This number tells you how long the sun’s UVB rays would take to redden your skin if you apply the sunscreen properly as compared with the amount of time without sunscreen. So if you use an SPF 30 product properly, it would take you 30 times longer to burn than if you used no sunscreen. Simultaneously, SPF 30 blocks approximately 97% of UVB rays. Higher numbered SPFs block slightly more of the sun’s UVB rays, but no sunscreen can block 100% of the sun’s UVB rays.
The US Food and Drug Administration has also concluded that the maximum SPF value on sunscreen should be “50+” as there is insufficient evidence to conclude a true difference in protection between products that are SPF 50, 75 and 100.
Water-Resistant. Dermatologists also recommend you look for the words “water resistant”. This tells you that the sunscreen is capable of staying on wet or sweaty skin for a longer while before you need to reapply. “Water resistant” tends to last for up to 40 minutes and “Very Water-Resistant” tends to stay for up to 80 minutes. For any case, sunscreens are not 100% waterproof and sweatproof and will still need to be reapplied.
Other tips when using sunscreen:
Be extra cautious near water, snow and sand. In these conditions, damaging rays of the sun tend to reflect more and increase your chances of sunburn.
Avoid tanning beds. Ultraviolet light from these sources tend to increase your risk for skin aging and skin cancer.
Consider a self-tanning product. If you choose to look tanned, do incorporate the use of sunscreen.
Perform regular skin-self exams. When in doubt, seek consult with your board-certified dermatologist.
TYPES OF SUNSCREENS
There are many available sunscreens on the market. To understand which one suits you best, we must first understand the type of UV rays.
There are two types of UV light that is capable of harming your skin – UVA and UVB.
UVB rays are responsible for producing sunburn. UVA rays on the other hand penetrate more deeply into the skin and cause premature skin aging such as wrinkling and age spots. Too much exposure to either UVA or UVB can cause skin cancer.
Sunscreens contain active ingredients that help prevent the sun’s UV radiation from damaging your skin. Here are two types of sunscreens and how they work for you:
Physical (Mineral) Sunscreen Ingredients
Some examples of these are titanium dioxide and zinc oxide. These ingredients block and scatter rays before they can penetrate your skin.
Chemical Sunscreen Ingredients
Some examples of these are oxybenzone, avodenzone and octisalate. These ingredients absorb UV rays before they can damage your skin.
Broad-Spectrum Protection
Broad-spectrum sunscreen is used to describe sunscreens that can protect you from both UVA and UVB rays. It would be wise to choose a sunscreen that can provide the greatest amount of protection from both types of UV radiation.
ISSUES ABOUT VITAMIN D
Will using sunscreen decrease your skin’s production of Vitamin D?
According to a Position Statement on Vitamin D by the American Academy of Dermatology, the AAD recommends that an adequate amount of Vitamin D should be obtained from a healthy diet that includes food rich in Vitamin D, foods/beverages fortified with Vitamin D and/or Vitamin D supplements. Vitamin D should not be obtained from unprotected exposure to UV radiation.
In this way, you can meet the required vitamin D you need without increasing your risk for skin cancer. If you are concerned about not getting enough Vitamin D, discuss your options with a board-certified dermatologist.
References:
American Academy of Dermatology
The Skin Cancer Foundation (skincancer.org)
AAD Position Statement on Vitamin D (2008, 2010)
Telemedicine in dermatology or teledermatology is a service provided by dermatologists to educate and communicate with the new and follow-up patients. It is conveniently located in the virtual realm. Physical travel is not needed unless the dermatologist specifies the need or urgency. A big plus for teledermatogy, is the way the distance is shortened, while still maintaining professionalism of an actual face-to-face in-clinic consultation.
Patients can seek consultation at the safety of their work, home or private spaces using a gadget of choice, whether cellphone or computer. Synchronous or face-to-face in video conference, asynchronous forwarded photographs, or both can be utilized.
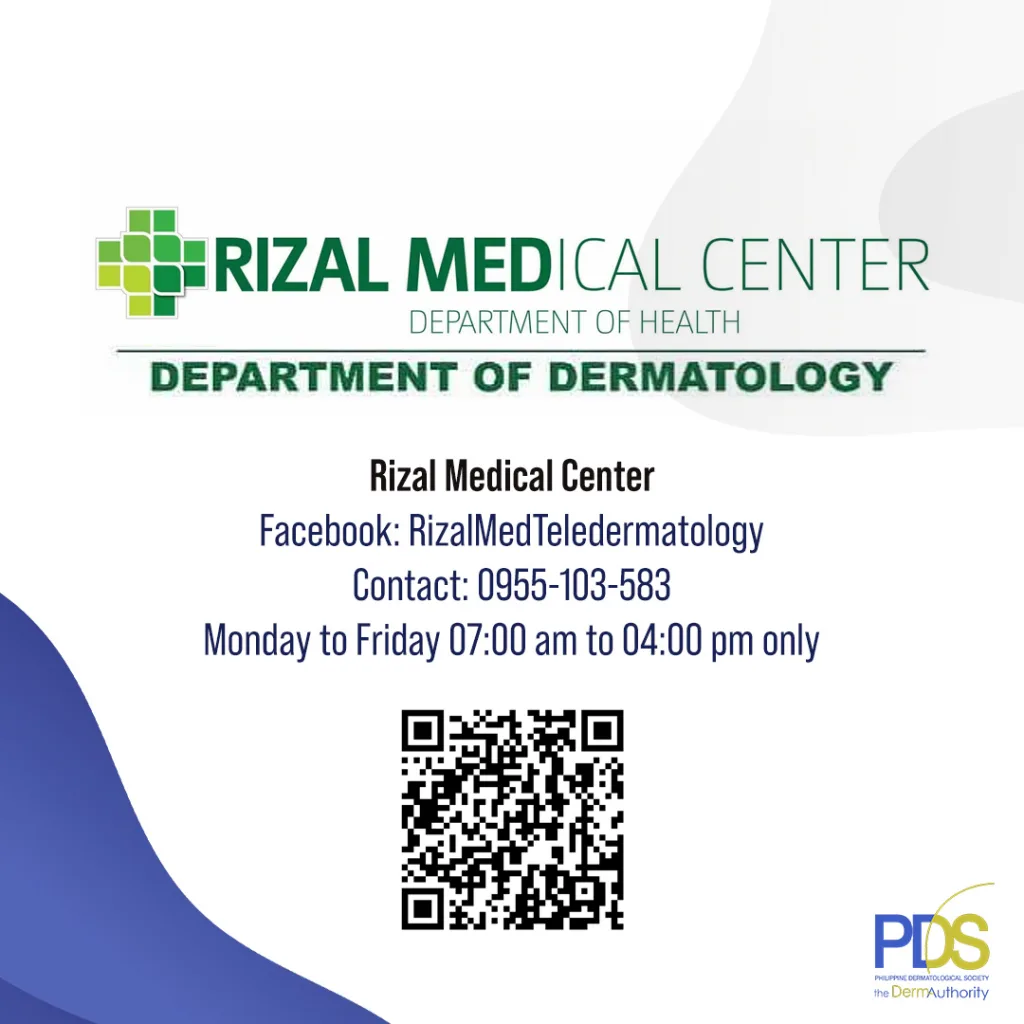
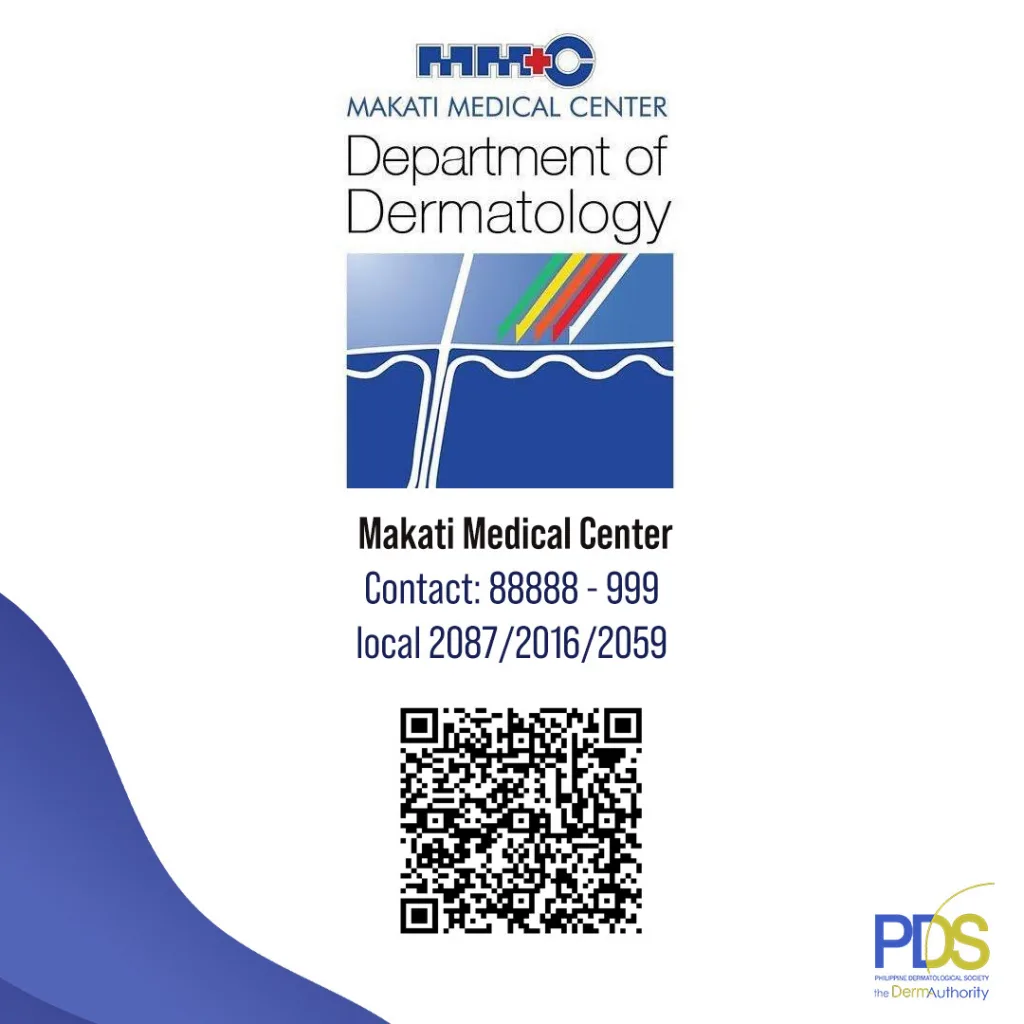
At present, there are 12 PDS accredited institutions and 3 applicant institutions giving FREE teledermatology services thru resident dermatologists in training.
Schedules are available, mostly from 7-5pm Mondays to saturdays.
Here are some information about the FREE teldermatology consults being conducting in the 12 training institutions. Feel free to contact them!








The 4th Annual meeting of the Asian Society of Dermatopathology (ASD) was organized by the Dermatopathology Society of the Philippines in the Philippine Dermatological Society (DSP-PDS). The event was held virtually on October 24-25, 2022 and was well-attended by multi-nationalities of over 195 registrants composed of dermatopathologists, pathologists, and dermatology consultants and residents/fellows-in-training. There were 17 plenary speakers from 8 different countries of Europe, USA and Asia with 10 case discussion speakers from the Asian countries All of the speakers were of high-caliber and world-renowned experts in their subspecialties. The overall chair of the organizing committee was Arnelfa C. Paliza, MD, FPDS, President of DSP-PDS, and the scientific committee was chaired by Ma. Jasmin J. Jamora, MD, FPDS.
Here are some of the testimonials from the attendees:
“The meeting was fantastic! It was a great success!” – Yu-Hung Wu, MD, ASD President
“It was a nice a meeting. Great job!” – Suat Hoon Tan, MD, ASD Vice-President
“The speakers were top-notched leaders in dermatopathology.” – Thuy Phung, MD, ASD treasurer
“It’s a hard act to follow.” – Joyce Lee, MD, ASD Chair of Education Committee
The next ASD may not be able to have the caliber and number of speakers such as this”- Daisuke Tsuruta, MD, overall chair of upcoming 5th ASD Annual Meeting
“Many thanks for the academic feast.” – Sivaranjini Ramassamy, MD, delegate from India
“Thank you. I really enjoyed it. It was a great meeting. I love the platform. I look forward to next year’s one.” – Alexander Nirenberg, MD, delegate from Australia
Organizing Committee of the 4th ASD Annual Meeting together with Yu-Hung Wu, MD, President of ASD
Day 1 Plenary: Diagnostic clues in Medical Dermatopathology
1st row (L-R): Kara Melissa T. Culala, MD (moderator); Rosalie Elinitsas, MD (speaker); Dr. Jacqueline Junkins Hopkins, MD
2nd row (L-R): Dr. Joyce Lee, MD (moderator); Dr. Jennifer McNiff, MD (speaker); Dr. Jag Bhawan, MD
Day 1 Case Discussion
1st row (L-R): Dr. Bryan K. Guevara, MD (moderator); Chia Hui Yi, MD (speaker); Dr. Dongyoun Lee, MD (speaker)
2nd row (L-R): Dr. Sondang Mh Aemilia Pandjaitan Sirait, MD (moderator); Chao-Kai Hsu, MD (speaker); Lei Wang, MD (speaker)
Free communications with the Research Committee: Mara Therese E. Huber, MD (Chair) and Eileen Liesl A. Cubillan, MD (Member)
Day 1 Plenary: Challenging Dermatologic Infections
1st row (L-R): Arnelfa C. Paliza, MD (DSP-PDS president); Andrea Marie B. Mendoza, MD; Maria Isabel Beatriz L. Puno, MD (moderator)
2nd row (L-R): Nopadon Noppakun, MD (speaker); Johannes F. Dayrit, MD (speaker); Maria Franchesca S. Quinio, MD (moderator)
Day 2 Plenary: Tackling tumors and nails
1st row (L-R): Steven D. Billings, MD (speaker); Phyu P. Aung, MD (moderator)
2nd row (L-R): Maria Jasmin J. Jamora, MD (moderator); Mary Grace Anne A. Calvarido, MD (moderator)
Day 2 Case Discussion
1st row (L-R): Arnelfa C. Paliza, MD (DSP-PDS president); Andrea Marie B. Mendoza, MD; Erin Jane T. Santos, MD (moderator)
2nd row (L-R): Poonnawis Sudtikoonaseth, MD (speaker); Ikmal Hisyam Bakrin, MD (speaker); Daisuke Tsuruta, MD (speaker)
Ken Natsuga
Day 2 Plenary: Advances in Dermatologic Diagnostics
1st row (L-R): Tan Suat Hoon, MD (moderator); Yu-hung Wu, MD (speaker); Riza Milante, MD (moderator)
2nd row (L-R): Ken Natsuga, MD (speaker); John McGrath, MD (speaker); Shang-Ian Tee, MD (speaker)
3rd row (L-R): Maria Jasmin J. Jamora, MD (moderator); Werner Kempf, MD (speaker); Arnelfa C. Paliza, MD (DSP-PDS president)
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by itchy, inflamed patches of skin. Dermatologists play a crucial role in diagnosing and managing eczema, providing relief and improving the comfort of individuals experiencing this condition.
Dermatologists are trained to identify the signs and symptoms of eczema during physical examinations. They assess the patient’s skin, looking for redness, dryness, swelling, and scaling. Dermatologists also consider the patient’s medical history and potential triggers, such as allergies or environmental factors, to develop a comprehensive understanding of the condition.
Once diagnosed, dermatologists develop personalized treatment plans for eczema management. These plans often include the use of emollients and moisturizers to hydrate the skin and restore its barrier function. In cases of severe eczema, dermatologists may prescribe topical corticosteroids or immunomodulators to reduce inflammation and alleviate itching. They also provide guidance on lifestyle modifications, such as avoiding known triggers and maintaining proper skincare routines.
In addition to treatment, dermatologists offer essential education to individuals with eczema. They explain the chronic nature of the condition and teach patients how to identify and manage flare-ups effectively. Dermatologists also discuss strategies for itch relief and the importance of maintaining healthy skin hygiene to prevent secondary infections.
To summarize, dermatologists play a crucial role in managing eczema and improving the comfort of individuals with this condition. By accurately diagnosing eczema, providing personalized treatment plans, and offering education, dermatologists empower patients to take control of their eczema symptoms and enhance their overall well-being.