Value at your desk. Contact Us
Corazon Almira Mella, MD, DPDS
Hair loss among women remains a “taboo” topic. Unlike with men wherein it is considered socially acceptable with advancing age, women carry the pressure of maintaining a full scalp of hair throughout life. The notion that hair is associated with one’s beauty, as old-fashioned as it seems, still encompasses today’s culture. But just like men, women also suffer from hair thinning and hair loss – medically termed as female pattern hair loss (FPHL). And, it’s about time the discussion on such topic be normalized – because the more women are aware of it, the more that they can take control. Moreover, the earlier the hair loss is acknowledged and addressed, the better the outcome will be.
What is female pattern hair loss?
FPHL is the most common cause of hair loss among women. It can affect any age group but is more widely seen after menopause. It is characterized by progressive and widespread thinning of hair over the top of the head or crown. Dermatologists refer to this as the “Christmas tree” pattern but the younger generation have termed it is as hair or scalp cleavage. In contrast with male hair loss, female pattern hair loss does not usually result in total baldness. The process usually occurs in bouts – wherein there are accelerated periods of hair loss of around 3-6 months that are followed by episodes of stability that can last a year.
What causes female pattern hair loss?
Now, there are many reasons for female hair loss and this not only includes FPHL but also other medical conditions, physical and emotional stress. To be able to rule out other possible causes, a consult with a board certified dermatologist should be done.
The condition has a strong genetic predisposition and these genes could be inherited from either or both parents. Unlike with male hair loss, it is not clear whether or not androgens or male sex hormones play a role in its development. Environmental factors such as psychological stress, hypertension, diabetes mellitus, smoking, lack of photoprotection and physical activity have also been noted to be possibly related to FPHL.
Are there diagnostic tests that needs to be done for female pattern hair loss?
To properly investigate the root cause of hair loss, several tests are done by the dermatologist. This may include a hair pull test which is done by gently pulling one’s hair to evaluate how many hairs come out, blood examinations to check for vitamin, mineral and hormone levels as well as scalp examination and trichoscopy to rule out other causes of hair loss. In select cases, a scalp biopsy might also be done by a dermatologist. Biopsies are done to exclude more other types of hair loss such as scarring alopecias (scarring alopecias leads to permanent hair loss).
What is the treatment for female pattern hair loss?
Although there is no absolute cure for female pattern hair loss, there are several treatments available. These treatments are mainly done to slow down or stop the progression of hair loss and not to promote hair regrowth, in general. Thus when getting treatment, it is important to manage expectations. Treatment outcome may also be quite variable.
Treatment options are classified to either topical or systemic. When it comes to topical medications, the most well-known is Minoxidil. Minoxidil was initially used to treat hypertension; but, over time, people who used Minoxidil noted hair growth areas in their body where they had lost hair. Studies have confirmed that application of Minoxidil can induce hair growth. However, it should not be regarded as a quick fix because it will take 4-6 months before improvement in hair density is noted. Furthermore, the use of the medication might actually cause more hair fall during the first few months of use. Another readily available topical treatment is Ketoconazole. Ketoconazole is recognized as an antifungal medication; however, it also has anti-androgenic properties that can be significant in controlling the hormones implicated in hair loss.
Aside from those mentioned, there are other forms of topical treatment – platelet rich plasma therapy, microneedling, and low level light therapy. These options may be presented to you by your dermatologist during consult.
Systemic treatment mainly involves the use of prescription medications such as Spironolactone and Finasteride. Unlike in male pattern hair loss, the use of these oral medications for female pattern hair loss have yet to receive approval from the FDA. The use of these medications should be done with precaution as they are not safe to use for pregnant women or women who are planning to get pregnant.
It might seem like a novel idea, but hair transplant can also be an option for females suffering from hair loss. Dermatologists who have been trained in hair transplant can provide appropriate counseling and assessment on whether or not a person is a good candidate for hair transplant.
Indeed, hair loss in women is not a topic often talked about and a lot of women still suffer in silence. However, it is time to discard the perception that hair loss only happens in men. Female pattern hair loss is not as uncommon as one thinks. There are board certified dermatologists available to help women go through such battle.
They are best qualified to counsel such patients and give proper advice on treatment options.
Reference:
Yip, L. et al. Female pattern hair loss. https://dermnetnz.org/topics/female-pattern-hair-loss. Jul. 2015.
Bhat, Yasmeen Jabeen et al. “Female Pattern Hair Loss-An Update.” Indian dermatology online journal vol. 11,4 493-501. 13 Jul. 2020, doi:10.4103/idoj.IDOJ_334_19
Singal A, Sonthalia S, Verma P. Female pattern hair loss. Indian J Dermatol Venereol Leprol. 2013 Sep-Oct;79(5):626-40. doi: 10.4103/0378-6323.116732. PMID: 23974580.
By: Bernadette Lou Caluya, MD, DPDS
What is Shingles?
Shingles is a skin condition characterized by grouped vesicles with a reddish base in a band-like distribution usually affecting just one side of the body.
What causes Shingles?
Shingles is caused by Herpes Zoster Virus (HSV), which is also the virus that causes chickenpox. Shingles occur in people who already had chickenpox at one point in their lives. When a patient is healed from chickenpox clinically, HSV goes into a “resting” mode or latent mode in the neurons. When the same patient’s immune system experiences a decline, this virus can reactivate and can cause the expected skin lesions on the areas of the body supplied by the affected neurons.
Who gets Shingles?
Anyone can get Shingles but the following groups of people have increased risk in acquiring the disease
– elderly
– immunocompromised individuals (organ transplant patients, cancer patients)
– patients with immune-mediated conditions (systemic lupus erythematosus, rheumatoid arthritis etc.)
– patients undergoing chemotherapy, immunomodulators and corticosteroids
– HIV patients
What are the physical findings?
The lesions usually start as red patches on the affected body part in a unilateral distribution. After 12 to 24 hrs, grouped vesicles form on top of the patches. On the 3rd day, these vesicles can be filled with pus. In 7 to 10 days, brown crusts can form on top of the lesions. These crusts can persists for 2 to 3 weeks
What are the other signs and symptoms?
Is it infectious?
YES, Herpes Zoster Virus infection is infectious. A patient can transmit it to other people through direct contact with the vesicles until 7 days from the initial appearance of the skin lesions. It can also be airborne in some cases. The people who have exposure with patients with Shingles won’t develop Shingles, they will develop chickenpox.
It is important for patients to avoid exposure to pregnant mothers, elderly people, newborns and children.
Is it treatable?
YES, HZV infection is treatable.
– ORAL ANTI-VIRAL MEDICATIONS
It is important to seek consult with a dermatologist once the skin lesions are noted. Anti-viral medications are effective if given during the first 72 hours of the disease. It is proven that anti-viral therapy can decrease the duration and severity of the skin rash and associated pain. It also prevents the appearance of lesions to other parts of the body.
– TOPICAL TREATMENT OPTIONS
-can be beneficial during the acute phase to relieve pruritus and pain. It can also hasten the drying of
skin lesions
What are the possible complications?
Is there a vaccine available?
Zostavax ® (live attenuated Oka/Merck strain VZV zoster vaccine) is available and recommended to adults >60 y/o of age for prevention of herpes zoster and its complications, especially post-herpetic neuralgia.
Dr. Mara Padilla Evangelista-Huber, FPDS, FDSP, MClinRes
What gives color to our skin?
Melanin is the pigment molecule that gives our skin, hair and eyes color. It provides protection from ultraviolet radiation, which can cause premature skin aging (wrinkles, uneven skin) and skin cancer.
Melanin is made by cells in the skin called melanocytes, and one of the crucial steps involves an enzyme called tyrosinase. After melanin is made, it is transferred from melanocytes to the keratinocytes (skin cells).
What is hyperpigmentation?
Hyperpigmentation refers to excess pigmentation. This pertains to areas of skin that appear darker in color compared to other regions. It may develop anywhere in the body, may be small patches or be more widespread. While hyperpigmentation is not generally harmful, it can be a symptom of an underlying medical condition.
What causes hyperpigmentation?
There are many causes for hyperpigmentation. These triggers basically tell the melanocytes to make more melanin. One of the most common causative factors is sun exposure, which is why sun protection is very important.
Causes of hyperpigmentation:
Individuals with medium to darker-colored skin types are more prone to develop hyperpigmentation compared to those with lighter skin types because the former have more melanin to begin with.
What are the types of hyperpigmentation?
The most common types of hyperpigmentation are melasma, post-inflammatory hyperpigmentation, and sun spots or solar lentigines.
Melasma is one of the most common reasons for consultation with a dermatologist. The hyperpigmentation is usually on the face, specifically on the forehead, cheeks, nose, chin, but can occur elsewhere. Melasma mostly affects adult women and darker skin types. It can be caused by hormonal changes (e.g. pregnancy, use of oral contraceptives).
Post-inflammatory hyperpigmentation. This type of hyperpigmentation occurs after inflammation (common in acne and eczema patients) and injuries. You’ll see dark patches of skin on previously inflamed or reddish areas,
Sun spots or solar lentigines. This type of hyperpigmentation occurs in areas with high sun exposure like the face, forearms, hands. These are flat, round to oval dark patches, may be single or appear in a group.
How do we prevent and treat hyperpigmentation?
When dealing with hyperpigmentation, a two-way strategy is recommended: (1) to protect the skin and prevent hyperpigmentation from developing, and (2) to treat and correct existing hyperpigmentation.
Sunscreens, sun protection measures and topical anti-oxidants like vitamin C are very helpful in preventing hyperpigmentation. The cause of hyperpigmentation (e.g. acne, eczema, insect bites) must also be addressed.
When it comes to treating hyperpigmentation, a combination of these methods are beneficial: one is to inhibit tyrosinase (an important step in melanin synthesis), another is to inhibit the transfer of melanin from melanocytes to keratinocytes (skin cells), and lastly, to increase the renewal of skin so that new skin cells can replace the old, hyperpigmented skin cells.
Protect and prevent:
Treat: inhibit melanin transfer
Treat: tyrosinase inhibitor
Treat: increase cell renewal
What is hydroquinone?
Hydroquinone is a prescription-only drug considered a standard in the treatment of hyperpigmentation. While effective when used correctly, it may cause irritation, burning, stinging, and dryness – with higher concentrations posing higher risks. It is not recommended to use hydroquinone continuously due to the risk of ochronosis (paradoxical hyperpigmentation). The use of hydroquinone is only advised under the guidance of a dermatologist.
How long will it take for hyperpigmentation to resolve?
It depends. Hyperpigmentation may go away even without treatment within 3 to 24 months, but treatment can speed up the process. Hyperpigmentation may fully resolve or lighten considerably, but for others it may not completely disappear.
Hyperpigmentation: a final word
References:
Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3(7):20-31.
Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7(8):13-17.
Vashi NA, Wirya SA, Inyang M, Kundu RV. Am J Clin Dermatol. 2017 Apr; 18(2):215-230.
Huerth KA, Hassan S, Callender VD. Therapeutic Insights in Melasma and Hyperpigmentation Management. J Drugs Dermatol. 2019 Aug 1;18(8):718-729
Katrina Canlas-Estrella, MD, FPDS
Diet is frequently associated in various skin disorders. One way in which diet affects skin disorders is the concept of food allergy. Food allergy is defined by the US National Institute of Allergy and Infectious Diseases as: “an adverse health effect arising from an immune response that occurs reproducibly on exposure to a given food”. Simply put, this occurs when there is a breakdown of the body’s tolerance to food ingested1,2. Typical manifestations of a food allergy are skin reactions such as hives and itchiness, respiratory tract symptoms such as difficulty of breathing, and gastrointestinal tract symptoms such as vomiting and diarrhea. A severe and potentially fatal reaction called anaphylaxis, can also be experienced. While many advances have been made in understanding the mechanism, treatment and prevention of food allergy, the mainstay of treatment remains to be avoidance of the food allergen/s1-5.
Allergenic foods comprising more than 85% of food allergy are egg, milk, peanut, tree nuts (walnut, cashew, pistachio), fish, shellfish, sesame seed, soy, and wheat. Several studies identify egg allergy as the most prevalent4,5. In adults, allergies to certain fruits and vegetables are common3. Usually, many people outgrow their food allergies over time, such as hen egg and cow milk allergies. In contrast, peanut and tree nut allergies, along with shellfish allergy, are known to persist throughout life1-3. In addition, nickel is also a very common allergen and this could be found in certain foods such as oatmeal, beans, peas, soybeans, shellfish, and chocolate2,4,6.
A hypoallergenic diet is a diet composed of foods low in allergenicity. Specifically, it is free from soy, nuts, egg, dairy, corn, beef, gluten, shellfish, and citrus fruits. That said, patients on a strict hypoallergenic diet should be carefully monitored and properly managed so as to avoid nutritional deficiencies. In children, food allergies to milk, egg, soy, and wheat tend to disappear during late childhood and these specific foods may eventually be tolerated after 1 to 2 years. As mentioned, allergies to peanut, tree nuts, and shellfish typically persist and may be lifelong1-4.
There are certain skin diseases that can benefit from a hypoallergenic diet. Several studies have shown that certain food allergens can lead to an exacerbation of a patient’s dermatitis. Specifically, food allergy has been shown to be present in 20 to 80 percent of patients with atopic dermatitis (AD). Thus, a hypoallergenic diet may be helpful in patients with AD. Other skin diseases that may benefit from a hypoallergenic diet are systemic contact dermatitis (SCD) and allergic contact dermatitis (ACD). Furthermore, acute vesicular hand dermatitis may benefit from a diet low in nickel-rich foods2,4,6.
In order to find out if one has a food allergy and identify the specific food/s one is allergic to, one may consult with an allergologist. A detailed history and thorough physical examination are important, then skin prick testing (SPT) or radioallergosorbent test (RAST) can be done to identify potential food allergens. Once potential allergens have been identified, one must always be vigilant in checking food labels and ingredients in order to prevent the unfortunate manifestations of food allergy. In the event of an allergic reaction, rescue medication should always be available1-6.
References:
Kaimal, Sowmya, and Devinder Thappa. “Diet in Dermatology: Revisited.” Indian J Dermatol Venereol Leprol, vol. 76, no. 2, 2010, pp. 103–116.
by: Maria Elinor Grace Q. Sison, MD, FPDS
What is keratosis pilaris?
Keratosis pilaris or “chicken skin” is a common condition due to plugging of the follicles of our skin. It is common in children and can improve by late adolescence but is often persistent. It is strongly associated with several skin conditions such as ichthyosis vulgaris and atopic dermatitis. The cause of keratosis pilaris is not well understood.
How does keratosis pilaris present?
Keratosis pilaris presents with small bumps with varying degrees of redness. It affects lateral cheeks, extensor aspects of the upper arms, thighs, and buttocks. In children the face and arms are mainly involved while in adults the lesions are found in extensor arms and legs.
How is keratosis pilaris diagnosed?
Diagnosis is made through physical examination by the dermatologist based on the appearance of the lesions and their distribution.
What are the treatment options for keratosis pilaris?
Reference:Bruckner, AL. Keratosis Pilaris and Other Follicular Keratotic Disorders. In: Fitzpatrick’s Dermatology. 9th Ed. USA: McGraw-Hill.
By Dr. Coreen Copuyoc-Sampedro
Does wearing make-up ruin your skin? Back in the day, dermatologists were known to be against make-up or any form of cosmetic camouflage since many products then—think 80’s to early nineties —would cause a slew of unwanted effects such as acne, contact dermatitis, and hyperpigmentation. Instead, we would promote healthy natural looking skin sans any cosmetic product. However, the beauty and skincare market has grown exponentially and this preconception no longer applies. This not only means that the variety and number of products increased, but that many formulations have also gotten more sophisticated and safe. Going all-natural with just sunscreen on your face is definitely still a good way to go, but wearing make-up can actually work well with your skin if you know how to choose the right ones for your skin type. Aside from that, cosmetics actually help a lot of people as a confidence booster and as part of self-care. In fact, I am one such dermatologist that loves make-up almost (almost!) as much as skin care.
So how do you choose the right cosmetics for you? This is best figured out on a case to case basis but basically depends, first and foremost, on your skin type and the environment you’re in. If you have normal skin, almost any product may work well on you so just use the weather as your guide. Wearing oilier formulations may not work as well in a hot & humid environment such as in Manila for example, but these may be best for cold, breezy weather such as in Baguio. For those with oily skin, lightly formulated water-based foundations and medium-coverage powders may work best, provided that the skin is still hydrated. And for those with dry skin, oil-based formulas work best to camouflage anything but again, diligent hydration everyday is really the best way to ensure that make-up applies nicely. Combination skin is quite tricky because you will need to mix and match the products you use per area on your face. Creams or oil-based products applied on dry parts while lighter, more water-based products on the oily parts. Then lastly, the most difficult skin type to choose products for, is sensitive skin. The primary concern for sensitive skin would be avoidance of irritating or allergenic ingredients in make-up such as fragrances and parabens, while also choosing formulations that work well with your base skin type between oily, dry, or combination skin. I personally have sensitive, combination skin and have discovered that I like mousse or cream-gel formulations best, with light finishing powder on areas that are a bit oily.
At the end of the day, all of these are simply general guidelines and choosing your cosmetics will still depend on which ones are accessible to you and work well with your lifestyle and environment. Keep in mind though that the best foundation for make-up is still healthy, luminous skin. So I recommend allocating more time and budget for skin care and always remember to remove your make-up right when you get home. So, does wearing make-up ruin your skin? Well, the correct ones shouldn’t, and that’s the tea.
Jarische Frances S. Lao-Ang, MD, FPDS
Skincare is for everyone, but is it different between men and women? We’re all familiar with the saying “skincare is for all ages”, but how about skincare for all gender?
To find out, let’s first know the structural differences between male and female skin.
Now that we know the structural differences between men & women, must there be a difference when it comes to skincare?
Unique skincare need for men: Facial hair
by Michelle-Adeline Noche-Apacible M.D, FPDS
What You Need to Know about Moisturizing
by Michelle-Adeline Noche-Apacible M.D, FPDS
Why is it important to moisturize?
“I don’t need to moisturize because I only have oily skin.” This is just one of the many myths surrounding moisturizing. The most important truth you need to know about moisturizing is simple- it’s extremely important for the skin’s integrity and appearance. Moisturizers come in different types and contain various components but they mainly improve skin hydration and enhance skin barrier repair. They target the stratum corneum, the outermost layer in the epidermis, necessary for retaining hydration. Its structure is the most important contributor in the overall moisturizing level.
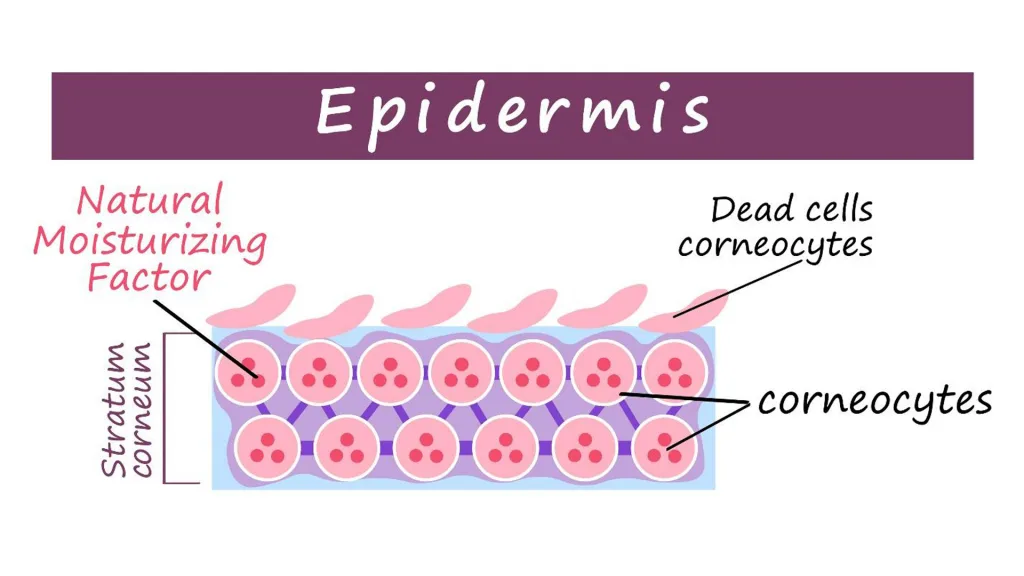
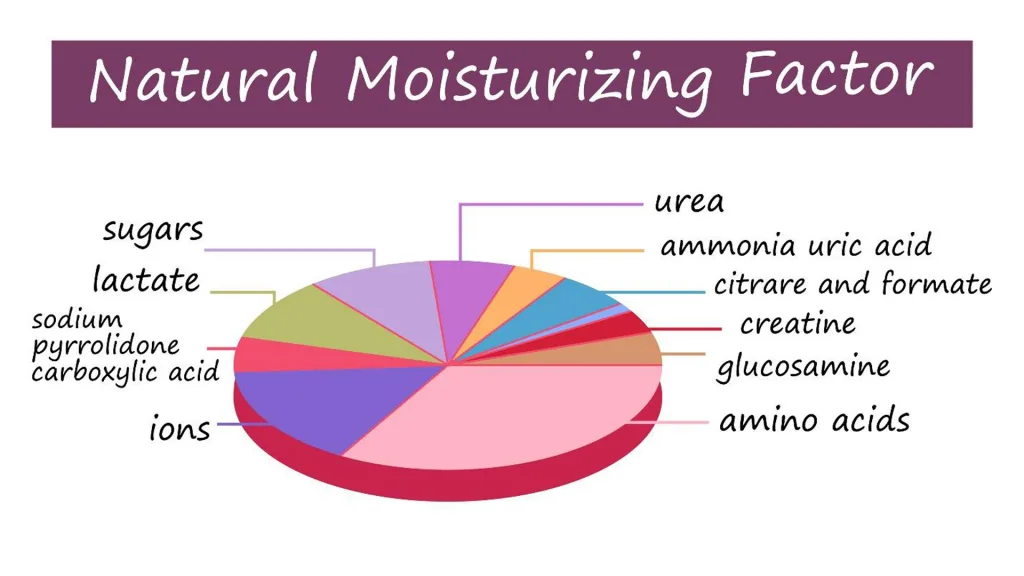
These involve four key processes namely corneocyte, stratum corneum lipid, natural moisturizing factor (NMF), and desquamation. All these processes aim to lead to the formation of an efficient moisture barrier. First, Corneocytes serve as the stratum corneum’s physical barrier by regulating water flux and retention. Next, stratum corneum lipids block external compound invasion and provide a barrier to water movement. Then, the natural moisturizing factor maintains the corneocytes’ hydration. Lastly, in desquamation, stratum corneum with a lack of moisture functions much less efficiently. This is why moisturizers step in to make sure that all these four processes are fulfilled.
When these processes are successfully carried out, the level of stratum corneum hydration significantly increases. Moisturizers do this by directly providing water to the skin and increasing occlusion to mitigate trans-epidermal water loss. Your skin’s appearance is positively affected because it smoothens the skin’s surface.
How do you choose the right moisturizer?
Choosing the right kind of moisturizer is not an easy task. It’s very easy to be overwhelmed with the sea of moisturizers being sold. Here are a few tips to find your skin’s match.
First, consider the factors that make a reliable moisturizer. These are particularly the natural moisturizing factor, ceramides and aquaporins (AQPs). Ceramides, a class of lipids, are essential building blocks of epidermal barrier structure. They also contribute to epidermal self-renewal and immune regulation. Aquaporins which come in many types contribute to water transport to the epidermis and hydration. For example, moisturizers with APQ3 spread both water and glycerol around the epidermis. It has also been proven to improve lipids’ metabolism which greatly contributes to the skin’s moisture.
Second, consider what your skin needs. Maybe if your skin is sensitive, you should avoid occlusives which can cause irritation. If your skin is dry, you should try a moisturizer with both an occlusive and humectant. This is because your skin may not have the protein-binding capacity to trap and retain moisture. Watch out for moisturizers with alcohols or fragrances as this may make your skin’s condition worse.
Lastly, consult with a board-certified dermatologist. Only a board-certified dermatologist will be able to recommend the most suitable moisturizer for your skin. They also have the necessary expertise in the different types of moisturizers and their respective mechanisms of action.
What are the kinds of moisturizers?
These usually come in three main kinds- emollients, occlusives, and humectants. Each has their own unique function that benefits your skin. Emollients, commonly used in topical pharmaceuticals, seal water into the skin. These provide a stronger skin barrier and appearance. Humectants on the other hand increase water absorption from the dermis into the epidermis where evaporation is easily possible. Occlusives have the most important effect when applied to wet skin since they prevent water from escaping the skin. These come in mineral oils, petroleum jelly and much more.
All of us have different skin types. Some people’s skin has a stronger ability to maintain moisture while others lack it. It is necessary for your skin’s health no matter the type. Moisturizers do this for you. Don’t let them sit in your vanity cabinets. Know what they do and integrate it into your skin care routine today.
Sources:
Visscher, M. O. (2003). Effect of soaking and natural moisturizing factor on stratum corneum water-handling properties. PubMed. https://pubmed.ncbi.nlm.nih.gov/12858228/
Coderch, L. (2003). Ceramides and skin function. PubMed. https://pubmed.ncbi.nlm.nih.gov/12553851/
Purnamawati, S., Indrastuti, N., Danarti, R., & Saefudin, T. (2017). The Role of Moisturizers in Addressing Various Kinds of Dermatitis: A Review. Clinical Medicine & Research, 15(3-4), 75–87. https://doi.org/10.3121/cmr.2017.1363
Draelos, Z. D. (2013, June 19). Modern moisturizer myths, misconceptions, and truths. PubMed. https://pubmed.ncbi.nlm.nih.gov/23837155/
Li, Q. (2019, December 5). The role of ceramides in skin homeostasis and inflammatory skin diseases. PubMed. https://pubmed.ncbi.nlm.nih.gov/31866207/
Boury-Jamot, M. (2009). Skin aquaporins: function in hydration, wound healing, and skin epidermis homeostasis. PubMed. https://pubmed.ncbi.nlm.nih.gov/19096779/
Smeden, J. (2016). Stratum Corneum Lipids: Their Role for the Skin Barrier Function in Healthy Subjects and Atopic Dermatitis Patients. PubMed. https://pubmed.ncbi.nlm.nih.gov/26844894/
Rawlings, A. V. (2004). Moisturization and skin barrier function. PubMed. https://pubmed.ncbi.nlm.nih.gov/14728698/
Jarische Frances S. Lao-Ang
What is a dermatologist?
A dermatologist is a medical doctor who specializes in managing skin, hair and nail conditions.
Dermatologists undergo several years of training to be able to help people. They take care of both adults and children. They manage not only eczemas and skin infections, but also cosmetic concerns.
What training does a dermatologist undergo?
What is a board-certified dermatologist?
After accomplishing the residency training, dermatologists take the diplomate board exam under the Philippine Dermatological Society (PDS). Once they pass the exam, they are board-certified dermatologists and are considered diplomate of PDS. They can now practice and hold clinics.
A person will be able to know if a practitioner is a board-certified dermatologist of PDS by looking at the attached DPDS or FPDS after their name. Aside from checking the names, one may verify by checking at the PDS website.
Subspecialty under dermatology
A dermatopathologist has one more year of training in pathology in which he or she is trained to identify biopsied skin samples under a microscope and make differential diagnosis of the skin concern involving the biopsied area.
An immunodermatogist is an expert in diagnosis and treatment of skin disorders characterized by defective responses of the body’s immune system. The most common immunologic skin condition are bullous diseases. They are also experts in evaluating immunofluoresnce readings for the correct diagnosis and treatment.
A photodermatologist has further training in UV-induced skin conditions and phototherapy (the use of UV light in managing skin conditions such as psoriasis, atopic dermatitis).
A dermatologic surgeon has expertise in doing surgical medical and cosmetic procedures.
Mohs surgery is a further subspecialty in dermatologic surgery where the expert performs surgery to manage skin cancer. It is a method wherein thin layers of skin are removed sequentially after examining in the microscope until the area is cancer-free. It aims to lessen the removal of normal healthy skin.
A laser specialist is an expert in using energy-based devices for managing skin conditions. They evaluate people and determine the recommended laser and wavelength to manage the particular skin concern.
A pediatric dermatologist is an expert in managing infants and children. Some conditions are encountered more in children such as a unique birthmark, vascular anomalies or neurocutaneous disease among others.
An environmental dermatologist specializes in the external triggers for skin irritation and allergy. They are experts in occupational and recreational related skin conditions and are also trained in performing clinic-based patch testing.
A leprosy subspecialty is an expert in handling and managing this mycobacterial infection.
STI experts are keen in diagnosing and managing sexually-transmitted condition. They handle cases such as syphilis, herpes, and HIV.
Why choose a board-certified dermatologist?
A board-certified dermatologist is a well-trained medical professional who gives evidence-based management to any skin, hair or nail concerns. It is best to seek consult with them for any skin concern for timely and proper treatment.
Dr. Carla Perlas, FPDS
What is Psoriasis?
A disease that is characterized by inflammation caused by dysfunction of the immune system also called immune-mediated disease which causes inflammation in the body. A raised plaques and scales on the skin are mostly the visible signs of the inflammation.
The World Health Organization (2014) classified psoriasis as a chronic non-communicable disease, emphasizing the distress caused by misdiagnosis, inadequate treatment, and stigmatization of this disease.
What causes Psoriasis?
Although the exact cause of psoriasis is unknown, several factors such as genetics, environmental triggers, and your immune system can all play a role. As a result, psoriasis is not contagious and cannot spread from person to person.
Because of the overactive immune system that speeds up skin cell growth, the immune system and inflammation play a role in psoriasis. Normal skin cells grow and shed in a month, but in psoriasis, skin cells grow and shed in only (3) three or (4) four days, and instead of shedding, the skin cells pile up on the skin’s surface whereas, the genetics of psoriasis are complex, and it is possible to develop psoriasis even if you have no family history of the disease, as well as a triggering event may cause a change in the immune system, resulting in the onset of psoriasis symptoms, this may vary from person to person, and what may worsen your psoriasis may have no impact on someone else.
Common psoriasis triggers include;
A great way to learn about your unique set of triggers is to track them over time. Keeping records of your symptoms and triggers can help you anticipate and treat your flares.
Locations and Types of Psoriasis
Psoriasis can appear anywhere on the body even on the scalp,face ,skin folds, hands, feet and nails. Plaques can be a few small patches or can affect large areas and it’s also possible to have psoriasis plaques and scales in more than one location on the body at a time.
There are five types of Psoriasis
Plaques typically appear symmetrically on the body, affecting the same areas on the right and left sides of the body. Plaque psoriasis frequently coexists with nail psoriasis, which manifests as discoloration, pitting, or separation of the nail from the foreskin.
What are the treatment used for Psoriasis?
The type and number of treatments involve are determined by the severity of your psoriasis that is determined by how much of your body it covers.
Finding the right psoriasis treatment and understanding the severity of your psoriasis and different treatment options can help you and your dermatologist work toward meeting your treatment goals. This includes the following;