Value at your desk. Contact Us
The Ospital ng Maynila Medical Center – Department of Dermatology has successfully completed its 22nd Dermatologic Surgical and Medical Mission last January 8-10, 2025 in Banaue, Ifugao.
This initiative, led by esteemed Dermatologist Dr. Ida M. Tiongco, an active faculty and consultant at the New York Presbyterian Hospital/Weill Cornell Medical Center and an active visiting consultant of the Ospital ng Maynila Medical Center, reflects our department’s unwavering dedication to providing high quality medical and surgical care to our indigent highland brethren.
Dr. Tiongco, who has partnered with the Good News Clinic and Hospital (GNCH) for the past 25 years, collaborated with its current director, Dr. Carol Abayao for this year’s mission. Together with the steadfast support of GNCH’s former director, Dr. Antonio Ligot, and his wife, Sylvia Ligot, the 22nd iteration of the apolitical Dermatologic Surgical and Medical Mission commenced.
A team of distinguished Board certified Dermatologists from the Philippine Dermatological Society, including Dr. Ma. Jasmin Jamora, the current President, Dr. Ma. Encarnacion Legaspi, current Board Member, Dr. Benedicto Carpio, OMMC Dermatology Department Chair, Dr. Gina Eubanas, and Dr. Odette Alonzo, helped complete the roster. They were likewise joined by Dr. Linda Valdelleon, former Dean of the UERM – College of Medicine and Surgery, and OMMC Dermatology residents Dr. Leanna Caylao, Dr. Reinard Wilopo, Dr. Tricia Amora, Dr. Eloisa Lobo, Dr. Michael Gunawan, Dr. Leonard Cua, and Dr. Jhudielle Eusebio, and SIMC Dermatology Chief Resident Dr. Janine Lovino-Ty.
Months prior to the event, Dr. Tiongco herself meticulously prepared surgical instruments and essential medical supplies, and ensured the safe transportation of the said supplies from the United States to the Philippines. Additional medications were generously provided by the Philippine Dermatological Society.



Figure 1. The Good News Clinic and Hospital Chapel converted into a consultation area.
On the morning of January 8, 2025, the team began the mission after a lengthy but scenic 12-hour journey to Banaue, Ifugao. The hospital chapel was converted into a consultation area, the delivery room into a four-bed operating room, and the patient rooms into electrocautery stations. Over the course of two and a half days from January 8 to 10, the team managed a total of 364 patients. Meanwhile, a total of 158 dermatologic surgical procedures were performed, consisting of 84 electrosurgical procedures, 38 excisions, 7 snip excisions, 22 intralesional steroid injections, 5 skin punch biopsies, and 2 incision and drainage procedures. The surgical diagnoses included Dermatosis Papulosa Nigra, Verruca Vulgaris, Seborrheic Keratosis, Acrochordons, Sebaceous Cysts, Ganglion Cysts, Lipomas, and various Nevi. Twenty patients whose provisional diagnoses included Systemic Lupus Erythematosus, Tuberculosis Verrucosa Cutis, and Melanoma had their samples sent for further dermatopathologic examination. Lastly, the most common dermatologic diagnoses during medical consultations were Pityriasis Versicolor, Seborrheic Dermatitis, Acne Vulgaris, Atopic Dermatitis and Scabies Infestation.




Figure 2. Images of the Dermatologic Surgical Team performing procedures on the patients of Banaue, Ifugao
Throughout the mission, Dr. Ida Tiongco and the volunteer Dermatologists provided an adequate venue for service learning, ensuring that the dermatologic needs of the community are met, while providing a venue where dermatologic surgical skills can be taught. Dr. Encarnacion Legaspi also shared her expertise in cosmetic procedures, particularly demonstrating techniques for repairing earlobe keloids.
During the Fellowship Night of the Banaue Medical Mission, a special moment was dedicated to celebrate the birthday of a distinguished guest volunteer, Dr. Jasmin Jamora, President of the Philippine Dermatologic Society (PDS). Amid an evening filled with camaraderie and celebration, Dr. Jamora presented two prestigious awards—the PDS Diamond Award and the PDS Award of Distinction for Humanitarian Service—to Dr. Ida Tiongco, in recognition of her more than 20 years of dedicated service in organizing dermatologic surgery and medical missions for underserved communities in Ifugao. Certificates of Appreciation were also given to Dr. Antonio and Sylvia Ligot, for their years of invaluable support to the current and previous missions.

Figure 3. Group picture to honor and celebrate Dr. Jasmin Jamora’s birthday during the Fellowship Night.

Figure 4. Awarding ceremony of the PDS Diamond Award and PDS Award of Distinction for Humanitarian Service to Dr. Ida Tiongco, and Certificate of Appreciation to, Dr. Antonio Ligot and wife, Sylvia Ligot.
This initiative was made possible through the support of Ospital ng Maynila Medical Center, particularly their Department Chair Dr. Benedicto Carpio, Department Training Officer, Dr. Eileen Regalado-Morales, and the rest of the OMMC Dermatology Consultant Staff, together with generous grants from the Philippine Dermatologic Society through PDS President Dr. Jasmin Jamora and contributions from Dr. Tiongco’s friends and relatives.

Figure 5. Group picture of the 22nd Dermatologic Surgical Medical Mission Team for January 8-10, 2025
All biopsy samples from the dermatologic surgical mission in Banaue, Ifugao, led by the Ospital ng Maynila Medical Center Department of Dermatology, have been meticulously documented and secured. As the team eagerly prepares for an upcoming review of the data, the Ospital ng Maynila Medical Center’s Department of Dermatology looks forward to unveiling a comprehensive analysis to bridge clinical observations with clinicopathological and demographic insights. This upcoming analysis report hopes to shed new light on dermatologic conditions in the region, providing valuable insight for future missions. Stay tuned for the exciting findings!

Figure 6. The 22nd Dermatologic Surgical Medical Mission Team at the Banaue Rice Terraces Viewpoint in Banaue, Ifugao
With the success of this year’s mission, the organizers look forward to future endeavors, ensuring that more communities across the Philippines gain access to essential dermatologic care. The 22nd Dermatologic Surgical and Medical Mission Trip stands as a testament to what can be achieved through collaboration, dedication, and the shared goal of making healthcare accessible to all.
Dr. CAROLYN CHUA-AGUILERA, MD, FPDS is a graduate of St. Luke’s College of Medicine. She finished her dermatology residency at Jose R. Reyes Memorial Medical Center and subspecialty training for Nail Pathology and Surgery at the Hospital of University of
Pennsylvania, Philadelphia and Hospital of University of Berne, Switzerland. She is a fellow of the Philippine Dermatological Society and an active consultant at St. Luke’s Medical Center Global City.
Trimming your nails may seem like an ordinary day-to-day activity, like brushing your teeth or combing your hair. But did you know that doing it incorrectly is the most frequent cause of ingrown toenails? Having this condition may be forgettable to some, but unforgettable to others because of the pain; it could cause enough pain for one to have a hard time walking, or sometimes, even standing.
So what is an ingrown toenail? It is a common condition wherein the side of the toenail grows down into the skin. The ingrown toenail may irritate the skin on the side of the toe, which can lead to swelling and redness; the affected area may then feel tender and warm to touch. Overtime, bleeding and draining of pus with secondary bacterial infection may ensue. It is most common to have ingrown toenail in the big toe.
Aside from incorrect trimming of the nails, an ingrown toenail may develop from wearing ill-fitting shoes and having poor foot hygiene. Repetitive trauma or foot injury from getting stepped on or banging your toe increases your chance. Those born with abnormally shaped nails, prone to excessive sweating, and those who are genetically predisposed have a higher possibility of ingrowing. It seems that anyone, really, may suffer from having an ingrown toenail. Those who are at higher risk include adolescents, athletes, patients taking certain medications like some chemotherapeutic drugs, and those with chronic diseases like diabetes, thyroid, cardiac, and
renal problems.
An ingrown toenail is best treated by a board-certified dermatologist, who will be able to assess and tailor-fit the treatment plan to the unique condition of the patient. Most of the time, an ingrown toenail can be managed conservatively by using simple yet effective techniques, without going through surgery. However, in severe cases, surgery may be the best option. Surgical removal of a part of the nail with application of a chemical to kill the nail root can be done to avoid recurrence. Usually, this procedure is done on children who keep getting an infection from ingrown toenails or to those who are genetically predisposed to having an ingrown toenail.
Prevention rather than cure is what they say and avoiding an ingrown toenail is very possible. Start with cutting your fingernails and toenails straight across and don’t round the corners. Though it might be a chore, it is better that you cut your own nails. After cutting, remember to
file the nail to smooth out uneven edges. Lastly, wear shoes that fit correctly and keep away from any form of trauma. If you suffer from chronic diseases like diabetes, it is best that you follow foot care recommendations from your doctor.
Trimming your nails may seem like an ordinary day-to-day activity, like brushing your teeth or
combing your hair. But did you know that doing it incorrectly is the most frequent cause of
ingrown toenails? Having this condition may be forgettable to some, but unforgettable to others
because of the pain; it could cause enough pain for one to have a hard time walking, or
sometimes, even standing.
So what is an ingrown toenail? It is a common condition wherein the side of the toenail grows
down into the skin. The ingrown toenail may irritate the skin on the side of the toe, which can
lead to swelling and redness; the affected area may then feel tender and warm to touch. Over
time, bleeding and draining of pus with secondary bacterial infection may ensue. It is most
common to have ingrown toenail in the big toe.
Aside from incorrect trimming of the nails, an ingrown toenail may develop from wearing ill-
fitting shoes and having poor foot hygiene. Repetitive trauma or foot injury from getting stepped
on or banging your toe increases your chance. Those born with abnormally shaped nails, prone
to excessive sweating, and those who are genetically predisposed have a higher possibility of
ingrowing. It seems that anyone, really, may suffer from having an ingrown toenail. Those who
are at higher risk include adolescents, athletes, patients taking certain medications like some
chemotherapeutic drugs, and those with chronic diseases like diabetes, thyroid, cardiac, and
renal problems.
An ingrown toenail is best treated by a board-certified dermatologist, who will be able to assess
and tailor-fit the treatment plan to the unique condition of the patient. Most of the time, an
ingrown toenail can be managed conservatively by using simple yet effective techniques, without
going through surgery. However, in severe cases, surgery may be the best option. Surgical
removal of a part of the nail with application of a chemical to kill the nail root can be done to
avoid recurrence. Usually, this procedure is done on children who keep getting an infection from
ingrown toenails or to those who are genetically predisposed to having an ingrown toenail.
Prevention rather than cure is what they say and avoiding an ingrown toenail is very possible.
Start with cutting your fingernails and toenails straight across and don’t round the corners.
Though it might be a chore, it is better that you cut your own nails. After cutting, remember to
file the nail to smooth out uneven edges. Lastly, wear shoes that fit correctly and keep away from
any form of trauma. If you suffer from chronic diseases like diabetes, it is best that you follow
foot care recommendations from your doctor.
Dr. CAROLYN CHUA-AGUILERA, MD, FPDS is a graduate of St. Luke’s College of Medicine.
She finished her dermatology residency at Jose R. Reyes Memorial Medical Center and
subspecialty training for Nail Pathology and Surgery at the Hospital of University of
Pennsylvania, Philadelphia and Hospital of University of Berne, Switzerland. She is a fellow of
the Philippine Dermatological Society and an active consultant at St. Luke’s Medical Center
Global City.
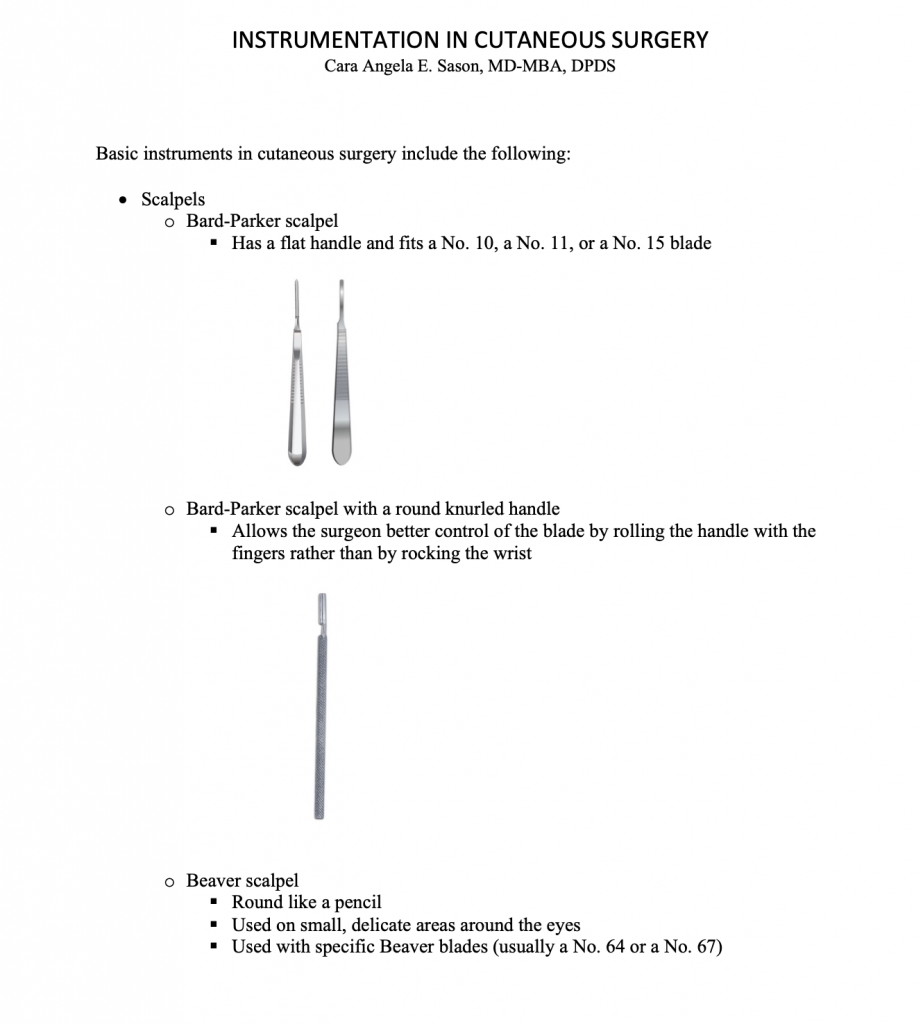
Master the art of dermatologic surgery with our acclaimed book, Practical Basic Dermatologic Surgery Volume 1 authored by our esteemed consultant, Dr. Ida Tiongco and the OMMC Dermatology alumni of batch 2021.
Limited copies left!
Elevate your skills with in-depth insights into surgical techniques. Unlock the secrets of dermatologic surgery procedures and stay ahead in the field. Order now for exclusive access to cutting-edge insights. Volume 2 coming soon!
Preview below!
For those interested, kindly fill out this google form:
For inquiries, please contact:
Over twenty members of the DSP PDS from across the country met up at Bueno Tapas & Wine Restaurant BGC, Taguig on January 17, 2024 to witness to the inauguration of the new diplomates of the society: Dr. Rosary Judielle Gucaban-Calimag, Dr. Lee-Ann C. Chang, Dr. Janelle G. Go, and Dr. Juan Paolo David S. Villena. The DSP-PDS toasted to another fruitful year under the leadership of Dr. Eileen Liesl A. Cubillan (President) and to welcome the successful board examination passers of 2023. The event was organized by Dr. Maria Franchesca Q. Calayag, the current Head of the Socials Committee.
Induction of diplomates 2023
(L-R) Dr. Mara P. Evangelista-Huber (Treasurer), Dr. Janelle G. Go (Diplomate), Dr. Juan Paolo David Villena (Diplomate) Dr. Lee-Ann Caro Chang (Diplomate), Dr. Rosary Judielle G. Calimag (Diplomate), Dr. Claudine Yap Silva (Head, CME) Eileen Liesl A. Cubillan (president)
Dr. Eileen Liesl A. Cubillan shares the accomplishments of the past year and the plans for the new one.



The skin as an immunologic organ has put at the forefront of the fastest and latest developments in the field of dermatology, with new insights of the pathogenesis, diagnosis, and treatment revolutionizing our field. As we navigate the world of immune-mediated skin conditions, we had the opportunity to learn from our very own Immunodermatology experts about the latest breakthroughs in research and updates on the management of common yet difficult to manage diseases during a special academic night.
Last September 6, 2023 the PDS Immunodermatology Subspecialty Core Group under the leadership of Dr. Clarisse Mendoza spearheaded the first ever Immunodermatology Masterclass in partnership with MIMS Philippines and through the educational grant from Pfizer. The event, held at Seda Bonifacio Global City, had a total of 100 attendees and 318 virtual attendees.

Current PDS President Dr. Cynthia Ciriaco-Tan opened the event and Dr. Marie Eleanore Nicolas served as the moderator for the sessions. The Masterclass was divided into two parts. The first segment was a series of lectures kicked off by Dr. Bryan Guevara’s “ADvancing therapeutic strategies for atopic dermatitis” where he highlighted the current advancements in the treatment of recalcitrant or severe atopic dermatitis, showed locally managed cases using the newer JAK inhibitors, and emphasized the importance of patient quality scores in evaluating treatment outcomes. This was followed by a talk by Dr. Mae Ramirez-Quizon entitled “Basics and breakthrough in alopecia areata.” Classic treatments as well as novel ones were discussed, including the JAK inhibitors which have highly improved treatment outcomes. Dr. Josef Symon Concha gave the lecture on “Targeted immunotherapy in improving treatment responses in vitiligo” where he highlighted the role of IL-15 in T memory cells responsible for relapses in vitiligo and the interferon-γ immunologic signature for vitiligo that is effectively inhibited by JAK inhibitors. Rounding off the first segment was Dr. Katrina Canlas-Estrella with “Approach to patients with chronic urticaria: Novel strategies for the stubborn welt and frustrating itch”, where she explained the tools used to evaluate chronic urticaria, advised on maximizing antihistamine use and updated the attendees on the guideline in the usage of omalizumab in patients with chronic spontaneous urticaria.
In between lectures the attendees enjoyed the quiz game Mentometer with the overall top three top takers both from the virtual and in-house attendees were given gift prizes for answering the fastest and garnering the highest points for correct answers. This was followed by an open forum after the first session where our experts answered interesting questions from the course participants.

The second part of the Masterclass was an interactive breakout room session where various cases were presented and participants could actively join and ask questions about the diagnosis and management of these immune-mediated skin disorders. Immunodermatology Subspecialty group members Dr. Cybill Dianne Uy (vitiligo), Dr. Jamaine Cruz (chronic spontaneous urticaria), Dr. Melanie Joy Doria-Ruiz (atopic dermatitis) and Dr. Johana Pauline Lazo-Dizon (alopecia areata) facilitated thought-provoking focus group discussions on vital, challenging topics commonly encountered by PDS Dermatologists in their practice.
It was indeed a successful academic exercise, for everyone. As we strive to provide better service and management to our patients, we continually update ourselves with the latest advancements that research offers. As the field of Immunodermatology continues to evolve, we look forward to conducting more Masterclasses in the future.
Shereen Reine S. Rodriguez-Gimarino, MD, FPDS
Because food is at the heart of Filipino culture, dietary restriction comes up as a frequent question during consults with the doctor. Much of our cuisine is flavorful, comforting, and tend to be on the greasy side. No wonder that after a trip to the doctor, we’d be told to cut down on certain foods to improve our health. We come to realize the role food plays in diseases, oftentimes leading to assumptions.
“I have pimples because I’ve been eating a lot of [insert food item] lately,” is a statement us dermatologists have heard too often. You may have been advised some time ago that they have nothing to do with each other. This is because in truth, the role of diet as a trigger for acne took decades to establish. Even with new research coming out regularly, the verdict for certain foods is still not absolute. In the midst of the abundance of anecdotes out there, evidence-based research updates are continuous, so here we are, setting the record straight with the evidence to date:
Food that promote acne:
1) Sugary foods (High glycemic index / glycemic load foods)
Glycemic index is a numeric score that indicates how rapidly a certain food is digested and elevates your blood sugar. The more refined and processed the carbohydrate is, the faster it metabolizes into glucose (high glycemic index). On the other hand, glycemic load is a ranking system that takes into account both the glycemic index of a food and the portion that you consume.
Several studies support that diets high in glycemic index / glycemic load exacerbate existing acne, and can prolong its duration. Therefore, be wary of products that are refined and those that have “added sugar” on the label. Consume foods rich in fiber, fat and protein because these release glucose more slowly, so they have a lower glycemic index.
2) Dairy
Consumption of cow’s milk – whole, low-fat and skim, has consistently been linked to acne exacerbation and break-outs in several studies, including an advisory from the American Academy of Dermatology. Interestingly, dairy products such as yogurt and cheese were not observed to influence acne.
3) Whey protein supplements
Commonly drank as protein shakes for body building and fitness, whey is the main protein component (80%) of milk. Dermatologists often encounter severe acne in protein shake drinkers. Supported by studies, severe acne in these patients persists even with appropriate medication, and respond only when whey protein is discontinued.
Food that protect from acne:
1) Low glycemic index / glycemic load foods
Just as how high glycemic index / glycemic load foods aggravate acne, low glycemic index / load foods reduce the inflammation, count and severity of acne consistently across multiple studies to date.
2) Omega-3 fatty acids and linoleic acid
These fatty acids, often associated with a Mediterranean diet and fish, have also been consistently observed to reduce inflammatory acne.
3) Vegetarian / vegan diet
Eating a fruit and vegetable-rich diet has been shown in recent studies to be acne protective.
Food that have been studied and deemed to not affect acne:
1) Salt
No association between salty food intake and acne was observed in studies.
2) Yogurt, cheese and other dairy products
As mentioned earlier, these milk products have no effect on acne in contrast to milk itself.
Food that have been studied but found to have insufficient evidence to either improve or aggravate acne:
1) Chocolate
This is food item is a popular question during an acne consult. Different studies varied in the brands and purity of chocolate (vs. its milk and sugar content) used, as well as the population involved, and have produced inconclusive results. Therefore, to date, chocolate is not yet proven to influence acne. Also be aware, however, that chocolates can easily become a high glycemic index food with dairy.
2) Probiotics
Probiotics have attracted attention for its gut health benefits over the recent years, and its effect on acne is not exempt from that. While initial studies are promising, further research and evaluation are needed to conclusively say it is beneficial for acne.
While there is some evidence supporting the relationship of acne and diet, this cannot replace proper evaluation of the cause of your acne and its corresponding management done in the setting of a Dermatology consult. Use the above information as a guide for your everyday food choices, rather than a treatment for your acne. Note that the evidence does not demonstrate that a certain type of food causes acne, rather they may influence existing acne positively or negatively.
Every year more and more evidences are unearthed about this topic, so stay tuned.
References:
by: Patricia Pontejos-Canivel, MD, DPDS
Acne is a hormonal skin condition that manifests as comedones known as “blackheads” or “whiteheads”. Comedones can become inflamed due to bacteria and turn into painful red bumps that become pustules or cysts. Our skin naturally produces oil or sebum and excess production can lead to clogging of the pores, this is what causes acne. Some factors that can contribute to the development or flaring of acne are:
When acne is left untreated, it can become severely inflamed and this can lead to scarring. Common types of acne scars are:
The best way to avoid scarring is to treat acne early and avoid picking on your skin. Different treatments can improve acne and acne scarring and this is best determined through a consultation with a board- certified Dermatologist. She/ he may suggest different treatments depending on the type of acne or acne scar you have.
“Maskne” or “Mask acne” is a new term that was coined due to the recent pandemic. It covers a wide range of skin conditions brought about by mask- wearing. Some cases may be real acne, but other conditions can also cause bumps on the skin. Some of these conditions are:
“Maskne” can be treated with proper diagnosis and treatment by a board- certified Dermatologist and should never be a reason to stop wearing masks in public. Some ways to prevent developing these conditions are:
Make sure to consult with a Board-Certified PDS Dermatologist!
REFERENCES:
Fitzpatrick’s Dermatology 9th edition
https://www.aad.org/public/diseases/acne/causes/acne-causes
by Katrina Canlas-Estrella, MD, FPDS
An allergic reaction is when a person’s immune system overreacts to an otherwise harmless substance (ex. Dust mite and peanut). In an allergic person, these substances are referred to as allergens. When a person is exposed to an allergen, his body produces antibodies that trigger the release of chemicals in the body like histamine, that causes the symptoms of allergies.
Allergic reactions vary, depending on several factors such as the allergen, the area of the body it affects, and the response of the person’s immune system. Symptoms can range from mild to severe. For example, food allergens can cause localized itching of the mouth, but they may also cause dangerous swelling of the tongue and the throat. Inhaled allergens like dust and pollen may cause itching of the eyes, sneezing, and wheezing. Some persons may be allergic to medications what can manifest as itchy rashes, hives, flushing of the skin, appearance of blisters, and swelling of the eyelids and the lips. Difficulty of breathing can occur in severe allergic reactions and can cause a potentially fatal condition called anaphylaxis.
Allergy can affect anyone. Some people are more prone to allergic problems when it runs in their family, while others may have no family history at all. People with other medical conditions such as asthma, eczema, chronic lung infections, and those with diseases that require intake of multiple drugs are more prone to developing allergies. Anything can be an allergen, Things that people are commonly allergic to include food (peanut, egg, soy, and shellfish), dust mite, tree and grass pollens, insect venom, medications, animal dander, and chemicals (hair dye, detergents).
Doctors can diagnose your allergies based on your symptoms. Your doctor may also perform tests (skin prick test, blood allergy test, and patch test) to find out what you are allergic to and how severe your allergies are.
Treatment depends on what your allergens are and how severe your reactions are to them. In general, you can avoid having allergic reactions by avoiding the allergens that cause them. Your doctor may recommend having an “allergy diary” and medications to relieve your symptoms. Allergists may recommend shots to certain allergens like dust and pollen.
A person with allergies should make a list indicating what he or she is allergic to and the type of allergy that he or she has. It is also helpful to inform their families, caregivers, schools, employees, and friends of what they are allergic to. Your doctor may also provide you with medications that you should carry with you at all times in case of an emergency. Early recognition of an impending allergic reaction will also prevent fatal complications.
by Michelle-Adeline Y. Noche-Apacible, FPDS
Atopic Dermatitis is commonly known to many as “eczema”, “asthma of the skin” or “hika sa balat.” Atopic dermatitis comes from the root word atopy or allergy. These can manifest as follows:
Infants from 0-24 months old: around the cheeks and outside parts of extremities. Just imagine the skin parts used when a baby crawls.
For 24 months old and above these manifest in flexural areas such as the skin on the inside of the elbows and knees.
Atopic Dermatitis is diagnosed through the use of criterias. Major criteria includes family history of allergy and recurrent skin condition. Minor criteria includes dry skin, keratosis pilaris (chicken skin), Dennie morgan folds (creases along the lower eyelids) etc.
The condition which involves increased IgE is usually inherited. This can present as allergic rhinitis (frequent sneezing in the morning), asthma or the same skin condition within the immediate or extended family members.
Patients often have dry skin since atopics lack the capability to retain moisture. Dryness causes pruritus (itch) can lead to severe scratching which damages the skin leading to infections. Atopics are also more prone to viral and fungal infections because their skin barrier is compromised.
Treatment starts with seeking a board-certified dermatologist from the Philippine Dermatological Society. Your Dermatologist will help you with finding the right moisturizer, maintaining a proper skin regimen, and avoiding bad habits.
Shorter baths periods with the proper moisturizer traps and retains the moisture preventing the escape of water from the skin. This prevents TEWL or Transepidermal Water Loss. Other further treatments may include proper use of topical corticosteroids, intake of antihistamines and prevention of secondary bacterial infections.
Although the journey in controlling your Atopic dermatitis may be frustrating, controlling and achieving a better daily life is definitely achievable. Most atopics are better by 17 years old. They then tend to get dry skin again when they approach their 40’s. An added fact: Did you know that most atopics have a high IQ?
So seek for a board-certified dermatologist now from the Philippine Dermatological Society and your journey to a better skin and quality life is on its way.
Sources (APA format):
American Academy of Dermatology Association. (n.d.). Eczema types: Atopic dermatitis diagnosis and treatment. Retrieved April 5, 2021, from https://www.aad.org/public/diseases/eczema/types/atopic-dermatitis/atopic-dermatitis-treatment
Md, A. P. S., & Md, A. M. J. (2015). Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence (5th ed.). Elsevier.
Allergic tendencies are associated with larger gray matter volumes
2018H Takeuchi, Y Taki, R Nouchi, R Yokoyama, Y Kotozaki, S Nakagawa, A Sekiguchi, K Iizuka, Y Yamamoto, S Hanawa, T Araki, CM Miyauchi, K Sakaki, T Nozawa, S Ikeda, S Yokota, M Daniele, Y Sassa, R Kawashima10.1038/s41598-018-21985-8Scientific Reports